Copper oxide coatings target multi-drug-resistant bacteria
Copper oxide nanoparticle coatings are being developed to reduce the risk of infection following surgery.
The research at Nottingham Trent University, UK, is inspired by concerns about increasing antibiotic resistance and over-reliance on antibiotics.
Dr Gareth Cave at the University highlights, 'Bacteria are evolving resistance faster than new antibiotics are being developed. Multi-drug-resistant (MDR) pathogens, such as Carbapenem-resistant Enterobacteriaceae (CRE) and Methicillin-resistant staphylococcus aureus (MRSA), are becoming more and more common. Unfortunately, most of us know someone, often a loved one, who has been affected by MRSA in a hospital.'
After using their nanoparticle technology to create the UK’s first, regulator-approved, antiviral, Type IIR face mask during the pandemic, the scientists have expanded the antipathogenic properties to include MDR pathogens, and developed the nanoparticles into a coating for use on materials in medical devices.
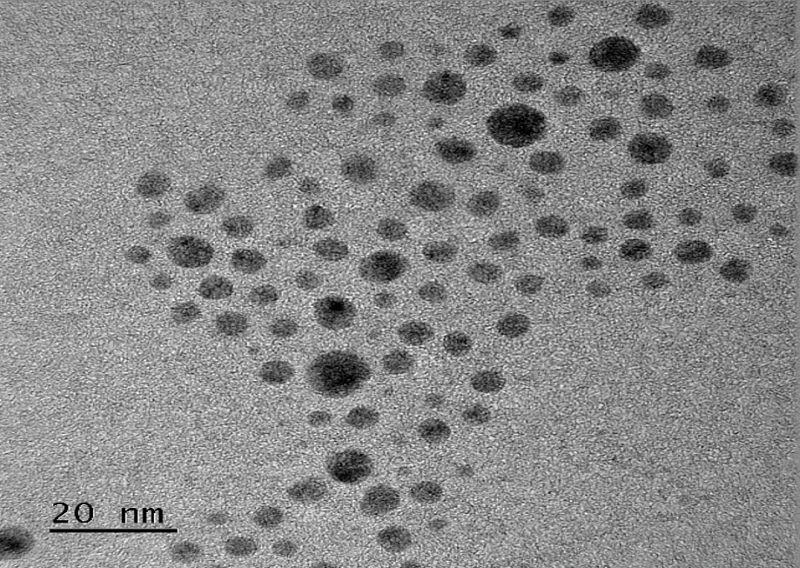
The coating is made from copper-oxide nanoparticles covered with amino acid and glutamic acid and held together by electrostatic interactions.
To develop the coating, a patented rotating-disk reactor controls the size, shape and uniformity of the nanoparticles. Amino acid is coupled to the surface of the nanoparticles, resulting in a complex that is dispersible in a solution as an ink.
Cave claims, 'This can then be applied to and bound to a surface, rendering it antipathogenic.'
The study finds that dip and spray coating methods exhibit antimicrobial activity, protecting against a range of clinically significant bacteria, including drug-resistant strains, while remaining non-toxic to human cells.
The range of bacteria repelled are gram positive and gram negative species and MDR pathogens, including Enterococcus faecium, Staphylococcus aureus, Staphylococcus epidermidis, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, Enterobacter species, Escherichia coli and Acinetobacter pittii.
In terms of repellence rates, E. coli sees a 99.8928% decrease in viable cells, while Acinetobacter pittii sees a 99.9967% decrease in viable cells. This equates to nearly a factor of 10 difference between the reduction of E. coli and A. pittii. Rates vary between these values from strain to strain.
Cave confirms the technology is currently being tested in dwelling and vascular catheters, endotracheal tubes, orthopaedic and dental implants, and prosthetics.
They currently have two patents for the material fabricaton and a third one describing the antipathogenic formulations and application.
This technology is already proven at scale, according to Cave. 'During the pandemic, we were able to manufacture three million face masks a day using similar technology and distributed them across the world. The same technology and process is also now used in the manufacture of heating, ventilation and air conditioning filters across the world.
They are now in 'open discussions' with medical device manufacturers to implement this technology into their devices, 'making them accessible globally'.