Surgical dressings to heal melanoma wounds
A graphene-oxide-protein material for dressings has healing properties for post-surgery melanoma patients.
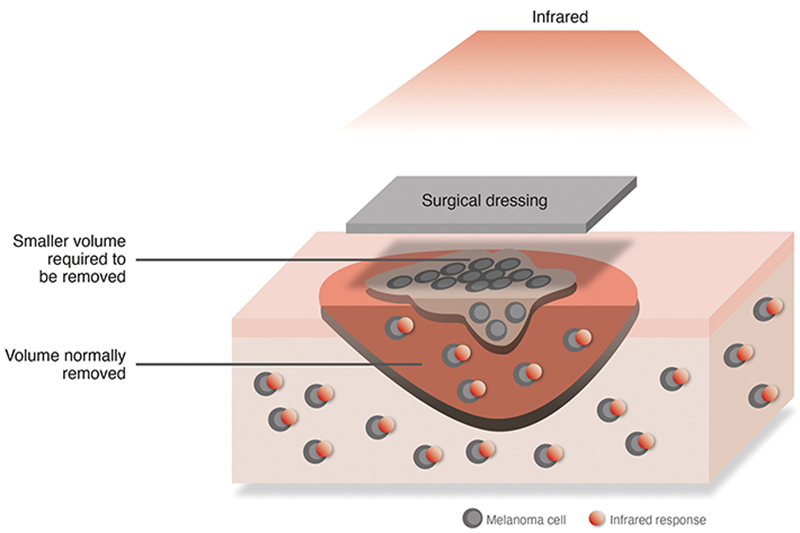
The material is designed to prevent the recurrence of cancer cells after the melanoma has been surgically removed, as well as to promote healing and healthy cell regeneration, according to the University of Nottingham, UK-led research project.
GO-elastin materials, which can be heated effectively at low temperatures so they become conductive, have been shown to promote the growth of immune-boosting endothelial cells.
Treatment for skin melanoma typically involves removing large sections of tissue, but cells can often return after an operation requiring further surgery, chemotherapy and radiotherapy. The cancer cells can also develop resistance to treatments.
Photothermal Therapy (PTT) is one of the new treatment options being explored by medical practitioners – the method enables materials to conduct heat by converting light.
Professor Alvaro Mata from the University of Nottingham explains that GO-protein materials offer potential for such biomedical devices. However, a major difficulty is that temperatures of more than 140°C are usually needed before the GO can conduct heat, which destroys the proteins and has restricted its medical use.
In a previous study published by the same University in 2020, the researchers created a self-assembled composite material that combines GO with the protein elastin for potential use in tissue engineering.
Mata shares, 'We found that when they are brought together in certain conditions, they spontaneously self-assemble into well-defined membranes and we don’t need any specialised equipment to fabricate them.'
This discovery provides the foundation for the team’s latest research, which starts with a reduction process to transform GO into graphene.
As Mata explains, finding a low enough temperature to successfully achieve reduction poses a significant challenge.
The team turned to ethanol for inspiration. '70% ethanol is known to efficiently penetrate the protein cage of bacteria and viruses, and has been shown to serve as an effective reagent to reduce GO,' he explains.
'If you have 100% ethanol, it can evaporate too quickly whereas 70% provides a balance between penetration and the solution’s maintenance before evaporation. We used this as a medium to penetrate into the nanoscale GO-elastin complexes and this enables the removal of oxygen-containing groups in an efficient manner while keeping the GO-elastin composite functional.'
An additional benefit of using the ethanol is that during the reduction process, the ethanol also sterilises the dressing.
According to Mata, the resulting material can be easily and efficiently heated with short exposures to near-infrared light (NIR) to a temperature of 85°C, which is just below the ethanol’s boiling point.
For this part of the study, the researchers partnered with Professor Tell Tuttle’s group at the University of Strathclyde, which used computing modelling to analyse the reduction process down to the molecular scale through simulation.
'There is another element here,' continues Mata. 'We know the GO-elastin material is conductive, but we also know from the first study that endothelial cells that make vascular tissue and are essential for the regeneration of tissue really like this material.'
This gave the researchers, led by Postdoctoral Fellow and Plastic Surgeon Yuanhao Wu, the idea of using GO-elastin material for melanoma patients.
The membrane can be used as a dressing and exposed to light from a NIR for short periods of time, which heats the material to a temperature that can kill cancer cells to prevent recurrence and promote the growth of endothelial cells.
Tests reveal the material only needs 15 seconds of light exposure every 48 hours. However, Mata adds that further funding is required to undertake larger-scale testing.
'I would envisage that people could use this at home right after surgery,' he suggests. 'They could have a patch where they expose it to NIR for 30 seconds or a minute every day.'