Flatworm’s suction inspires medical adhesive
A medical adhesive modelled on the structures found in marine animals like mussels and flatworms uses 'suction to absorb blood, clear the surface for adhesion and bond to human tissue to provide a physical seal', according to the Canadian-based scientists behind its development.
The material, made from both synthetic and naturally derived polymers, could help medical practitioners in hospitals and ambulances prevent trauma patients from haemorrhaging if applied to bloody wounds.
Lead author Guangyu Bao, a recently graduated PhD Student, explains that the inspiration came from marine animals, only after the McGill University researchers in Montreal first developed a hydrogel adhesive system that mimics the process slugs use to stick to substrates. This consists of two parts – a hydrogel adhesive matrix and a synthetic “bridging” polyacrylamide solution.
'Although we were able to achieve excellent adhesion performance, the process of preparing two parts during the application of our adhesive is not as spontaneous as the slug,' he explains.
'We wanted to streamline the application process and make our technology readily available. That’s when we started to look into marine animals that can also form adhesion underwater.'
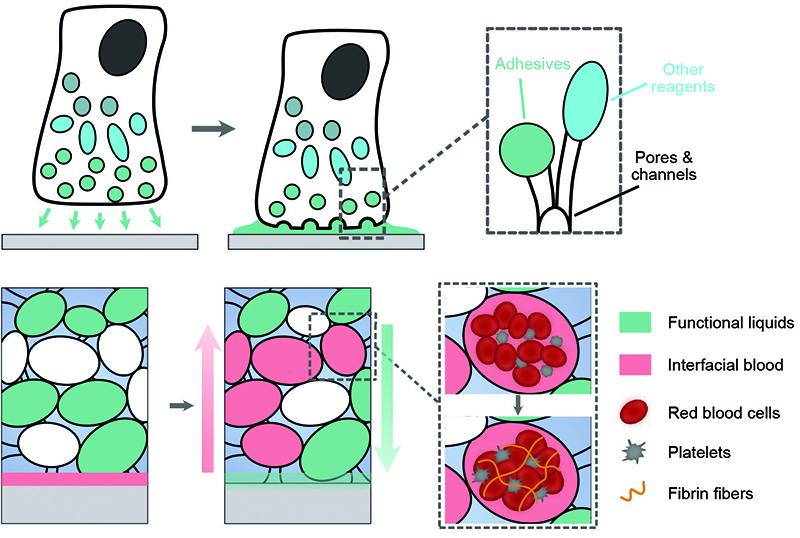
The researchers have found that flatworms and mussels contain structured porous spaces to store and secrete adhesive agents, thereby enabling adhesion underwater.
By incorporating these features into their original hydrogel adhesive matrix and loading the polymer solution inside, it accelerates adhesion formation using capillary suction.
Bao explains how the material is made using a 'double-network' design to synthesise a hydrogel that is both biocompatible and biodegradable, as well as being tough and highly stretchable. Next, the hydrogel is frozen at -20oC to create ice crystals inside the solution.
To form pores in the matrix, freeze-drying is employed to remove the ice crystals. The fabrication process is completed when the team loads the polymer solution into the dry and porous xerogel and partially fills the pores. The finished product can then be kept frozen for long-term storage or used immediately.
'We built xerogels, a dried format of hydrogels, with interconnected microstructures,' Bao explains.
'We partially impregnated those microstructures with an adhesive, functional liquid and left some microstructures dry. When our adhesives are applied to the bleeding site, the dry parts act as mini vacuums by providing capillary suction forces to rapidly absorb the blood, clearing the bleeding surface.'
Professor Jianyu Li, who supervised the research, notes that the team had to redesign the adhesive hydrogel matrix using chitosan after the original alginate-based hydrogel quickly lost adhesion. He says the substitution prolongs shelf life and also improves usability.
Another benefit is that chitosan is more stable inside the human body. The adhesive does not generate excessive stress nor compress surrounding tissues and nerves, even after it has been implanted, Li asserts.
Bao adds that laboratory tests on animal models have determined the material’s hemostatic efficiency in stopping blood loss, rapidly adhering to blood-exposed surfaces without the need for compression.
Bao adds that the matrix can also promote blood coagulation, which can offer an additional sealing benefit.
In a further development, the team says it can build advanced functions to provide better wound care.
'We can make our adhesive antimicrobial, reducing the chance of bacterial infection in the wound,' says Li. 'This is critically important in emergencies where a sterile environment is not immediately accessible.'
Tests have so far looked at how bleeding from liver injuries can be stopped, with plans to investigate injuries to arteries and other conditions.







